Table of Contents
Dementia and Alzheimer’s disease are among the most common forms of cognitive impairment in the aging population, presenting unique challenges to healthcare professionals and families alike. The complexity of these conditions necessitates a multi-faceted approach to care that addresses the medical, psychological, and social needs of patients. In evaluating Alzheimer’s vs dementia, effective treatment strategies are essential for managing symptoms, maintaining quality of life, and supporting both patients and caregivers. In this article, we explore the variety of treatment methodologies and the importance of customizing care to meet individual needs.
Understanding Dementia and Alzheimer’s Disease
Recognizing the early signs of dementia and Alzheimer’s disease is pivotal for timely intervention. Symptoms often start with mild memory loss and difficulties in cognitive functions, which eventually escalate to impairments that affect daily living. These can include disorientation, language problems, and changes in personality or behavior. Early detection is essential in managing diseases proactively and planning for future care.
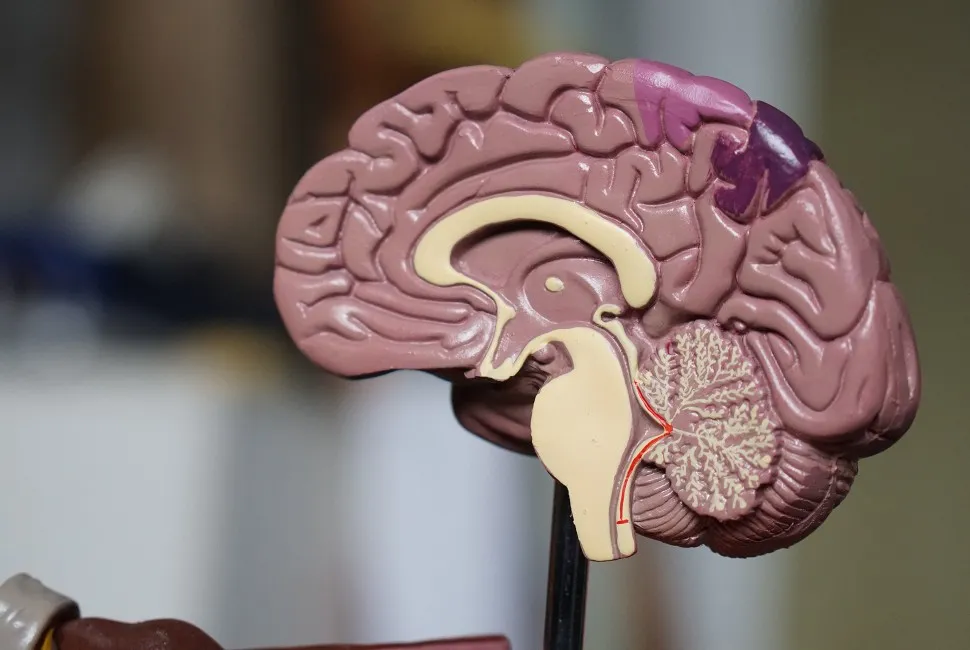
Diagnosing dementia and Alzheimer’s relies on a thorough medical assessment, including patient history, physical examination, and often neuropsychological testing. Brain imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scan can provide visual evidence of changes in brain structure associated with the diseases. Biomarkers are increasingly becoming a key diagnostic tool, helping to identify the disease in its early stages.
It is crucial to understand the distinction between Alzheimer’s disease and other types of dementia. While all Alzheimer’s patients have dementia, not all dementia is due to Alzheimer’s. This differentiation is important in developing tailored treatment plans that target specific symptoms and disease progression patterns unique to each type.
The Importance of Personalized Care in Dementia and Alzheimer’s Treatment
Personalized care is a cornerstone in the treatment of dementia and Alzheimer’s. As these conditions manifest differently in each individual, a one-size-fits-all approach is not effective. Personalized treatment plans may include a blend of medication, therapy, and support services, all tailored to the individual’s symptoms, disease stage, and personal preferences.
Understanding a patient’s personal history, lifestyle, and preferences can help in designing an intervention plan that minimizes stress and promotes comfort. For instance, incorporating familiar routines and activities into a patient’s daily schedule can help maintain a sense of normalcy and self. Moreover, accounting for a patient’s cultural background and language can significantly improve the effectiveness of care and communication.
A multidisciplinary approach involving doctors, nurses, therapists, and social workers is crucial in personalizing care. Collaboration among these professionals ensures that every aspect of the patient’s health and well-being is considered, promoting an optimal living environment. The role of caregivers is also essential; they often have insights into the patient’s preferences and behavior that can inform a more tailored care strategy.
Integrating Pharmacological Treatments with Lifestyle Management

Pharmacological treatments, such as cholinesterase inhibitors and memantine, have shown some success in managing dementia symptoms. These medications work by supporting the function of neurotransmitters in the brain, potentially improving cognitive function or delaying its decline. However, they are not curative and are most effective when combined with lifestyle management strategies.
Lifestyle management for dementia and Alzheimer’s patients may include a healthy diet, regular exercise, and cognitive stimulation. Ensuring a balanced intake of nutrients can contribute to overall brain health, while physical activity helps maintain mobility and cardiovascular health, potentially slowing disease progression. Cognitive stimulation activities, structured to match individual abilities, support mental engagement and can improve mood and self-esteem.
Cognitive Therapy and Memory Care Techniques for Patients
Cognitive therapy is a key element in treating dementia and Alzheimer’s patients. Techniques such as reality orientation, reminiscence therapy, and validation therapy can assist patients in retaining their sense of identity and connection to their environment. Such therapeutic approaches are designed to slow cognitive decline and enhance the patient’s current abilities.
Memory care techniques, such as the use of memory aids and prompts, can help patients navigate daily life by providing consistency and routine. Visual cues, lists, and the structuring of living areas can restore a degree of autonomy in performing everyday tasks. This can lead to significant improvements in self-confidence and a reduction in the frustration or anxiety associated with memory loss.
Support from professional caregivers trained in cognitive therapy and memory care can make a significant difference in the quality of care received. Specialists in cognitive therapy possess the skills to engage with patients in ways that are meaningful and respectful of the person’s experiences and cognitive level.
Overall, the treatment and care for patients with dementia and Alzheimer’s are complex and require careful consideration of each individual’s unique journey. Effective care balances medical interventions with therapeutic strategies to enhance quality of life. By embracing a tailored approach, healthcare providers, caregivers, and families can make a meaningful difference in the lives of those affected by these debilitating diseases.

Liam Stephens is a dynamic and skilled blogger, recognized for his ability to identify trends and create compelling content. As the founder of Remi-Portrait.com, Liam has become a reliable source of information across various fields such as food, technology, health, travel, business, lifestyle, and current events. He specializes in delivering up-to-date technology news and insights, catering to the diverse community that surrounds Remi-Portrait.com. His proficiency and engaging writing style have earned him a dedicated audience, solidifying his reputation in the digital sphere.